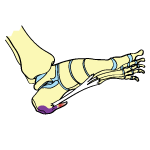
Heel Pain is usually felt underneath the heel or at the back of the heel. Heel Pain can be the result of an acute injury, but can also be caused by repetitive activities and overuse that puts a lot of strain on the heel.
Causes
Determining the cause of your Heel Pain can be difficult, as there are a variety of possibilities. Here are some of the more common cases of Heel Pain:
- Plantar Fasciitis
- Achilles Tendonitis
- Bone Bruise
- Heel Spurs
- Bursitis
- Stress Fracture
- Arthritis
- Tarsal Tunnel Syndrome
 Athletes who do a lot of jumping and landing from jumps are more prone to developing Heel Pain from the repeated stress on the fat pad underneath the heel.
Athletes who do a lot of jumping and landing from jumps are more prone to developing Heel Pain from the repeated stress on the fat pad underneath the heel.
Heel Pain in children is often attributed to Sever’s Disease, which occurs when the child’s heel bone grows faster than the other structures in the ankle and leg.
Heel Pain can also be the result of wearing improper shoes (such as flip-flops) or mechanical/gait issues (such as having flat feet).
Signs & Symptoms
Signs and symptoms associated with Heel Pain include:
- Pain under the heel bone
- Pain at the back of the heel
- Pain while walking
- Pain that comes on gradually
If your Heel Pain is associated with an injury, you may also have:
- Inflammation
- Bruising
- Tenderness
Treatment
In order for treatment to be as effective as possible, it will help to know the exact cause of your Heel Pain. If you haven’t already, you should see a healthcare professional to receive a formal diagnosis.
A good first step is to follow the RICE method — Rest, Ice, Compression, Elevation (especially if your Heel Pain is the result of an injury). Rest means trying not to put too much weight on the foot, and avoiding any activities that could cause further injury or strain. Applying Ice and Compression will help to bring down any swelling you have, as well as control the pain. Elevating your foot above your heart will work to alleviate any inflammation you may be experiencing.
If you need to take painkillers, consider taking an NSAID (non-steroidal anti-inflammatory drug) such as Advil or Aleve. Not only do NSAIDs help with the pain, they also work to reduce swelling. Just make sure you only take painkillers when you’re resting — taking painkillers when you’re active is a bad idea, as they completely block the pain signal, making you oblivious to any further damage you may be doing to your heel.
Depending on the cause of your Heel Pain, you may want to consider physical therapy. If you have Plantar Fasciitis or Achilles Tendonitis, your doctor may recommend physiotherapy sessions so you can restore strength and range of motion to the foot and ankle.
Taping the painful area can help provide you with extra support and stability, which is very helpful during the recovery process. Look for heel taping videos and application instructions online for ideas.
Sometimes the solution is as simple as investing in a pair of new, comfortable shoes. Make sure they are closed-toe, supportive shoes that are suitable for the activities you want to do. Shoes should never be too tight or too loose — shoes that fit properly are very important to foot health and mechanics.
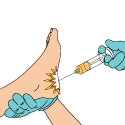
Cortisone shots should be your last resort before having surgery. Cortisone shots are designed to temporarily relieve pain and swelling, however, they come with various risks and side effects. This includes infection, bone death, skin discoloration and complete tendon rupture.
Surgery should only be considered if all other avenues of treatment have been exhausted. The type of surgery you undergo will depend on the cause of your Heel Pain, but there are various procedures for Plantar Fasciitis, Achilles Tendonitis, Bursitis, etc.